Banerjee, Amitava, Benedetto, Valerio  ORCID: 0000-0002-4683-0777, Gichuru, Phillip, Burnell, Jane
ORCID: 0000-0002-4683-0777, Gichuru, Phillip, Burnell, Jane  ORCID: 0000-0002-4601-1632, Antoniou, S, Schilling, R, Strain, WD, Ryan, R, Watkins, Caroline Leigh
ORCID: 0000-0002-4601-1632, Antoniou, S, Schilling, R, Strain, WD, Ryan, R, Watkins, Caroline Leigh  ORCID: 0000-0002-9403-3772 et al
(2019)
Adherence and persistence to direct oral anticoagulants in atrial fibrillation: a population-based study.
Heart
.
ISSN 1355-6037
ORCID: 0000-0002-9403-3772 et al
(2019)
Adherence and persistence to direct oral anticoagulants in atrial fibrillation: a population-based study.
Heart
.
ISSN 1355-6037
Preview |
PDF (Author Accepted Manuscript)
- Accepted Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. 798kB |
Preview |
PDF (Supplementary Material)
- Supplemental Material
Available under License Creative Commons Attribution Non-commercial No Derivatives. 761kB |
![Figure 1 [thumbnail of Figure 1]](https://clok.uclan.ac.uk/29866/3.hassmallThumbnailVersion/29866%20Figure%201%20Aug%202019.jpg) 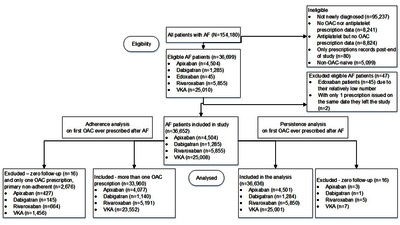 Preview |
Image (JPEG) (Figure 1)
- Supplemental Material
Available under License Creative Commons Attribution Non-commercial No Derivatives. 193kB |
![Figure 2 [thumbnail of Figure 2]](https://clok.uclan.ac.uk/29866/4.hassmallThumbnailVersion/29866%20New%20Figure%202.jpg) 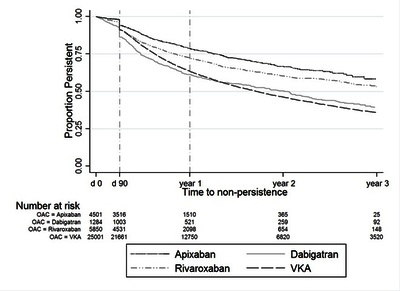 Preview |
Image (JPEG) (Figure 2)
- Supplemental Material
Available under License Creative Commons Attribution Non-commercial No Derivatives. 55kB |
![Figure 3 [thumbnail of Figure 3]](https://clok.uclan.ac.uk/29866/5.hassmallThumbnailVersion/29866%20Figure%203.jpg) 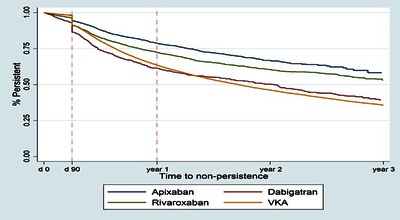 Preview |
Image (JPEG) (Figure 3)
- Supplemental Material
Available under License Creative Commons Attribution Non-commercial No Derivatives. 49kB |
Official URL: http://dx.doi.org/10.1136/heartjnl-2019-315307
Abstract
Background Despite simpler regimens than vitamin K antagonists (VKAs) for stroke prevention in atrial fibrillation (AF), adherence (taking drugs as prescribed) and persistence (continuation of drugs) to direct oral anticoagulants are suboptimal, yet understudied in electronic health records (EHRs).
Objective We investigated (1) time trends at individual and system levels, and (2) the risk factors for and associations between adherence and persistence.
Methods In UK primary care EHR (The Health Information Network 2011–2016), we investigated adherence and persistence at 1 year for oral anticoagulants (OACs) in adults with incident AF. Baseline characteristics were analysed by OAC and adherence/persistence status. Risk factors for non-adherence and non-persistence were assessed using Cox and logistic regression. Patterns of adherence and persistence were analysed.
Results Among 36 652 individuals with incident AF, cardiovascular comorbidities (median CHA2DS2VASc[Congestive heart failure, Hypertension, Age≥75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65-74 years, Sex category] 3) and polypharmacy (median number of drugs 6) were common. Adherence was 55.2% (95% CI 54.6 to 55.7), 51.2% (95% CI 50.6 to 51.8), 66.5% (95% CI 63.7 to 69.2), 63.1% (95% CI 61.8 to 64.4) and 64.7% (95% CI 63.2 to 66.1) for all OACs, VKA, dabigatran, rivaroxaban and apixaban. One-year persistence was 65.9% (95% CI 65.4 to 66.5), 63.4% (95% CI 62.8 to 64.0), 61.4% (95% CI 58.3 to 64.2), 72.3% (95% CI 70.9 to 73.7) and 78.7% (95% CI 77.1 to 80.1) for all OACs, VKA, dabigatran, rivaroxaban and apixaban. Risk of non-adherence and non-persistence increased over time at individual and system levels. Increasing comorbidity was associated with reduced risk of non-adherence and non-persistence across all OACs. Overall rates of ‘primary non-adherence’ (stopping after first prescription), ‘non-adherent non-persistence’ and ‘persistent adherence’ were 3.5%, 26.5% and 40.2%, differing across OACs.
Conclusions Adherence and persistence to OACs are low at 1 year with heterogeneity across drugs and over time at individual and system levels. Better understanding of contributory factors will inform interventions to improve adherence and persistence across OACs in individuals and populations.
Repository Staff Only: item control page

 Tools
Tools Tools
Tools https://orcid.org/0000-0002-4683-0777
https://orcid.org/0000-0002-4683-0777
